The Importance of a Night Routine for People with a Laryngectomy
The integration of a proper daily routine in the use of your HME can lead to a significant improvement in your quality of life.1 Your involvement in this is vital. This blog will guide you through the information you need to help improve respiratory symptoms after surgery.

The Importance of Sleep
In combination with a healthy diet and exercise according to your abilities, sleep is seen as essential to a healthy lifestyle. A good sleep improves your health and quality of life.2 It is quite common that people who have been through cancer treatment have poor quality of sleep.3
But what does poor quality of sleep really mean?
When talking about healthy sleep, it’s not only about sleep duration. It is very much about having a regular sleeping routine without interruption or disturbance.4
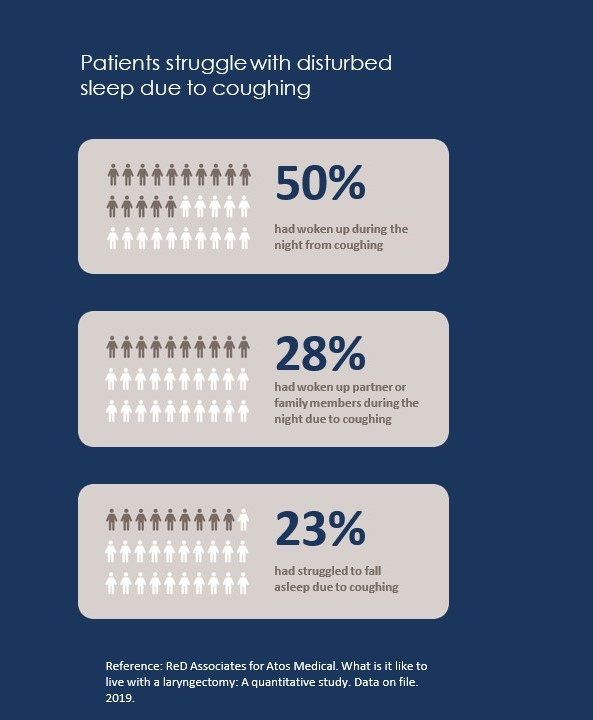
Sleep is disturbed because of coughing
Coughing at night impacts sleep quality for people with a laryngectomy and thus quality of life.5 Coughing wakes you up, depriving you of the rest you need.
The Function of Your Nose
As you are aware, you breathe exclusively through your stoma after a total laryngectomy. Your nose and its functions of humidification, heating and filtration of inspired air, are no longer involved in your breathing process.6 Keep in mind that improved sleep outcomes are associated with HME use due to reduced disruptions caused by coughing and mucus management. So, by using HMEs both during the day and the night, you can improve your sleep quality and pulmonary symptoms.1, 7, 8 Evidence shows that people can experience a decrease of pulmonary symptoms already after 2 weeks of adherent HME use.1
Day & Night Routine
Keep in mind that improved sleep outcomes are associated with HME use due to reduced disruptions caused by coughing and mucus management. So, by using HMEs both during the day and the night, you can improve your sleep quality and pulmonary symptoms.1, 7, 8 Evidence shows that people can experience a decrease of pulmonary symptoms already after 2 weeks of adherent HME use.1
Tips for a healthy sleep routine:9
- Be consistent. Go to bed at the same time each night and get up at the same time each morning, including on the weekends
- Make sure your bedroom is quiet, dark, relaxing, and at a comfortable temperature
- Remove electronic devices, such as TVs, computers, and smart phones, from the bedroom
- Avoid large meals, caffeine, and alcohol before bedtime
- Get some exercise. Being physically active during the day can help you fall asleep more easily at night.
To recap, a good night’s sleep is beneficial to your health in many ways. That’s why it’s important to report any issues or concerns you might have regarding sleep with your clinician. If you would like to know more about night HMEs, ask your clinician or connect with Atos Medical through your preferred channel of communication. Different shapes of adhesive that adapt best to your neck anatomy are available .Adhesives are made from different materials: Acrylic or hydrocolloids. All to adapt to your specific skin needs or preferences.
Explore our online learning platform for more valuable information.
If you have any questions or comments, do not hesitate to contact us below.
*required fields
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
References
1. Pierce RJ, Worsnop CJ. Upper airway function and dysfunction in respiration. Clin Exp Pharmacol Physiol. 1999;26(1):1-10.
2. Scheenstra RJ, Muller SH, Vincent A, Ackerstaff AH, Jacobi I, Hilgers FJ. A new heat and moisture exchanger for laryngectomized patients: endotracheal temperature and humidity. Respir Care. 2011;56(5):604-11.
3. Scheenstra RJ, Muller SH, Vincent A, Hilgers FJ. Heat and moisture exchange capacity of the upper respiratory tract and the effect of tracheotomy breathing on endotracheal climate. Head Neck. 2011;33(1):117-24.
4. Hilgers FJ, Ackerstaff AH, Aaronson NK, Schouwenburg PF, Van ZN. Physical and psychosocial consequences of total laryngectomy. Clin Otolaryngol Allied Sci. 1990;15(5):421-5.
5. Leemans M, van Sluis KE, Van Son R, Van den Brekel MM. Interaction of functional and participation issues on quality of life after total laryngectomy. Laryngoscope Investig Otolaryngol. 2020;5(3):453-60.
6. Parrilla C, Minni A, Bogaardt H, Macri GF, Battista M, Roukos R, et al. Pulmonary Rehabilitation After Total Laryngectomy: A Multicenter Time-Series Clinical Trial Evaluating the Provox XtraHME in HME-Naive Patients. Ann Otol Rhinol Laryngol. 2015;124(9):706-13.
7. Ward EC, Hancock K, Boxall J, Burns CL, Spurgin AL, Lehn B, et al. Post-laryngectomy pulmonary and related symptom changes following adoption of an optimal day-and-night heat and moisture exchanger (HME) regimen. Head Neck. 2023;45(4):939-51.
8. Bien S, Okla S, van As-Brooks CJ, Ackerstaff AH. The effect of a Heat and Moisture8 Exchanger (Provox HME) on pulmonary protection after total laryngectomy: a randomized controlled study. Eur Arch Otorhinolaryngol. 2010;267(3):429-35.
9. Zenga J, Goldsmith T, Bunting G, Deschler DG. State of the art: Rehabilitation of speech and swallowing after total laryngectomy. Oral Oncol. 2018;86:38-47.
10. van Sluis KE, van der Molen L, van Son R, Hilgers FJM, Bhairosing PA, van den Brekel MWM. Objective and subjective voice outcomes after total laryngectomy: a systematic review. Eur Arch Otorhinolaryngol. 2018;275(1):11-26.
11. ReD Associates, Quantitative Research. What is it like to live with a total laryngectomy. 2019
Share
Save to my content